1. Why is each patient hypoxaemic and what will happen when the FiO2 is raised to 1.0 (i.e. 100% oxygen therapy)? Precise answers cannot be calculated but assume reasonable values for unknown data.
Correct answer:
Patient 1:
This patient has a mild upper respiratory tract infection and no significant low respiratory tract pathology. However, he is probably hypoventilating due to gross obesity restricting normal respiratory movement. Assuming his gas transfer and V/Q matching are normal, his PaCO2 can be calculated from the alveolar gas equation (Chapter 14):
where P
AO
2≈P
aO
2 = 6.6 kPa (as measured); P
IO
2 = F
iO
2 × (barometric − water vapour pressure) = 0.21 × (101 − 6.2) = 19.9 kPa breathing air, and R, the respiratory quotient, is ~0.8. Thus, P
aCO2 = 10.6 kPa and if the arterial blood gas measurement confirms this, the patient has type 2 respiratory failure (Chapter 23). If the measured
aCO2 was much lower, it would suggest the assumptions were wrong and that another mechanism was causing or contributing to his respiratory failure.
When the patient is given 100% O2 (F
iO
2 1.0):
P
IO
2=F
iO
2 × (barometric – water vapour pressure)
=1 × (101–6.2)=95kPa
So:
P
aO
2 ≈ P
AO
2 = 95 –
10.6
/
0.8
=82kPa
Patient 2
This patient has a diffusion defect due to the interstitial lung disease (ILD, Chapter 30) although usually there is a significant contribution of ventilation/perfusion (V/Q) mismatch due to the hypoxaemia. His PAO2 is thus greater than his PaO2. Arterial blood gas (ABG) shows his PaCO2 is low (4 kPa). The substantial increase in PAO2 when this patient is given 100% oxygen (FiO2 = 1) will more than overcome the partial diffusion defect associated with the ILD, and if this were a pure diffusion defect the PaO2 could approach 90 kPa.
P
aO
2 = 95 –
4
/
0.8
=90kPa
Even allowing for a wider than normal range of V/Q ratios in this patient, there would still be a substantial increase in P
aO
2 on 100% oxygen.
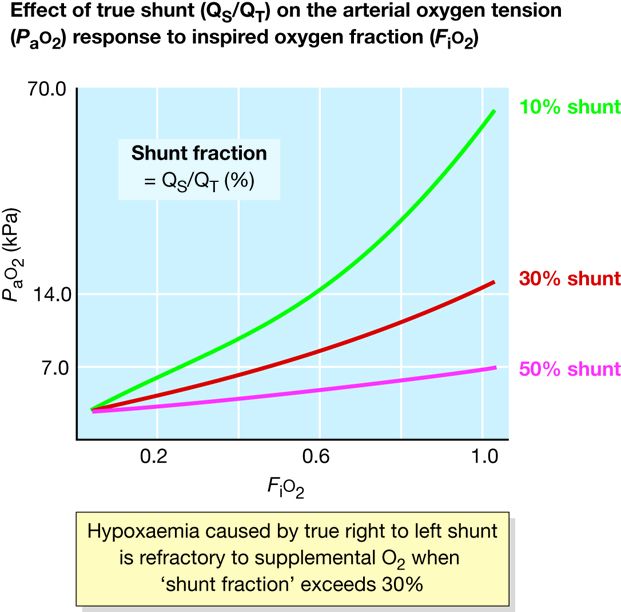 Figure 49
Figure 49 Effect of true shunt (Q
S/Q
T) on the arterial oxygen tension (P
aO
2) response to inspired oxygen fraction (F
iO
2).
Hypoxaemia caused by true right–to–left shunt is refractory to supplemental O2 when ‘shunt fraction’ exceeds 30%.
Patient 3
This patient is hypoxaemic due to true right–to–left shunting causing admixture of venous blood to systemic arterial blood (Chapter 13). As in the second case, the PAO2 will be 90 kPa with an FiO2 of 1.0. However, the saturation is already 100% in oxygenated blood passing through the lungs, and O2 content will not be substantially increased by the high PAO2 apart from the small quantity of O2 dissolved in blood (90 × 0.023 mL; Chapter 8). The blood shunted from right to left through the atrial septal defect remains unaffected by the increased PAO2 and acts as venous admixture lowering oxygenation in the systemic circulation. Consequently, an FiO2 of 1.0 only fractionally increases systemic PaO2 perhaps to ~7.5 kPa in this case.