A 70-year-old man presents with a 12-hour history of not being able to pass urine. He has had problems in the past with his ‘waterworks’ and has noticed that his stream is very slow and barely reaches the pan of the toilet. He has no significant co-morbidities. On examination he has a palpable bladder and his genitals are entirely normal. Examination of his prostate reveals a 60-g benign-feeling prostate. You diagnose him with acute urinary retention.
-
1. What catheter would you use and why?
Show Answer
Correct answer:
Using the principles set out in Chapter 17, Catheters, we can identify the correct catheter based on catheter size, number of channels, tip design and material.
- • Size: the patient is male so a 14–16 Fr catheter would be appropriate.
- • Channels: there is no haematuria so a three-channel catheter is not required. However, the catheter will need to stay in at least over night so a two-channel catheter is required.
- • Tip design: there is nothing in the history that suggests difficult catheterisation so a normal straight Foley tip catheter would be adequate. It is always a good idea to have a back up though.
- • Material: the catheter is likely to only need to stay in for a couple of days to a week before the patient will have a trial without catheter. Therefore a PTFE coated latex catheter would be ideal as they are common and can remain for up to 28 days, as long as the patient is not allergic to latex.
So, in summary, the patient needs a size 14–16 Fr, two-way Foley, PTFE catheter.
Two days later he returns to the hospital to have a trial without catheter. Unfortunately, he is unable to pass urine and develops supra-pubic discomfort and a palpable bladder. He needs a catheter while he awaits a definitive procedure in 6 weeks’ time.
-
2. Using the same principles as before, describe what catheter you would use?
Show Answer
Correct answer:
A 14–16 Fr, two-way Foley, hydrogel or silicone catheter, which can be kept in place for up to 3 months.
-
3. What definitive procedure is he going to have and what are the risks?
Show Answer
Correct answer:
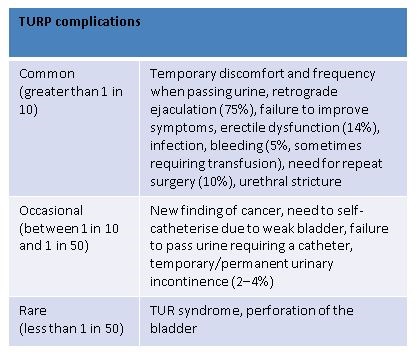
Transurethral resection of the prostate (TURP). The risks can be split into common, occasional and rare.
-
5. What factors were found to have an influence on the risk of developing TUR syndrome?
Show Answer
Correct answer:
The time of the resection (>90 minutes) and size of the gland (>45 g). The risk of TUR syndrome is reduced by using saline as an irrigant as is the case in bipolar TURP.