Other emergencies
Case 2: A Patient with Abdominal Pain and Weight Loss
CASE
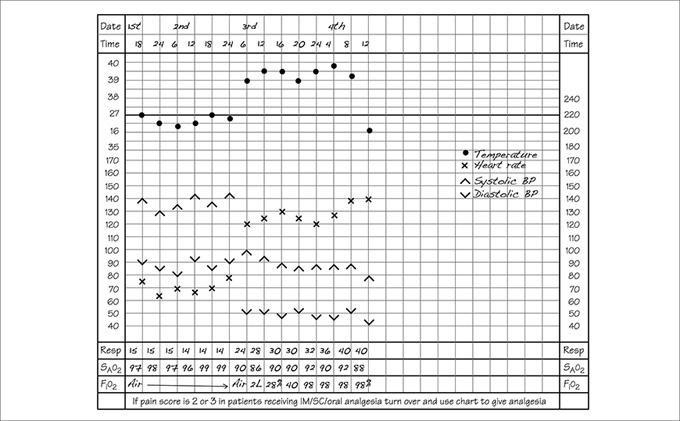
A 72‐year‐old woman presents with a 2‐month history of intermittent abdominal pain and weight loss of around half a stone which she attributes to poor appetite. She has noticed over this period of time that she has been more constipated, which she had put down to eating less. Her GP has referred her to A&E on Friday afternoon because the pain is worse in the last 24 hours and she is unable to keep anything down. She appears to be in pain and is vomiting. On examination her heart rate is 76 beats/min in sinus rhythm with a BP of 140/90 mmHg. Respiratory rate is recorded at 15 breaths/min and oxygen saturations are 99% on air. She is alert and orientated and able to give a good history of events. The abdomen appears distended and she is unsure when she last had her bowels open. Bowel sounds are present and there is no guarding or rebound. There is a suggestion of mass in the left iliac fossa. A nasogastric tube is inserted and the patient commenced on intravenous fluids. A CT scan is booked to investigate the abdominal findings further. The patient continues with fluid therapy over the weekend and analgesia in the form of morphine. She requires increasing amounts of analgesia as the pain is getting worse. You are called on the Monday morning by the ward staff as they are worried about her going down for her CT as she is ‘unwell’. Her observation chart is shown in Fig. 0001. On examining her abdomen there is evidence of guarding and rebound. She has become breathless and a chest X‐ray is performed which shows air under the diaphragm.
QUESTION 1
Your score this session: 0 of 0
What is the diagnosis when you review the patient?